Triathlete Injuries: Prevention, Recovery, and Performance Optimization
A Triathlete’s Guide to Injury Prevention and Recovery: How to Stay Healthy, Train Smarter, and Perform Your Best
Triathlon is one of the most demanding sports in the world. It requires athletes to push through grueling hours of training across three disciplines — swimming, cycling, and running — all while maintaining the endurance, strength, and resilience needed to perform on race day.
But here’s the reality most triathletes don’t like to admit: injury is more the rule than the exception.
Studies show that the overwhelming majority of triathletes — nearly 9 out of 10 — will face an overuse injury at some point during their training or racing journey. Most of these injuries strike not during competition, but in training, where the long hours and repetitive stress take their toll. And while some aches and pains fade with rest, the wrong injury, left unchecked, can derail months of progress and even end a season.
The good news? Most triathlon injuries are highly preventable and very treatable with the right approach.
This article breaks down the most common triathlete injuries, why they happen, and — most importantly — how you can train smarter, recover faster, and prevent setbacks so you can stay in the game and keep progressing.
Why Triathletes Are So Prone to Injury
Unlike single-sport athletes, triathletes face the challenge of balancing three distinct disciplines. Each discipline stresses the body differently, and the transition from one to the next creates unique strain patterns.
A few key reasons injuries are so common:
High training volume: Most triathletes train 10–20 hours per week, and Iron-distance athletes often go beyond that. Repetitive strain builds up quickly.
Imbalanced loads: The ratio of swimming, cycling, and running isn’t always balanced, leading to overdeveloped muscles in some areas and weaknesses in others.
Poor biomechanics: Small issues like a misaligned bike seat, faulty running gait, or shoulder mobility restriction can add up over thousands of training repetitions.
Fatigue: Long blocks of training without adequate recovery weaken tissues and increase the likelihood of breakdown.
The end result: overuse injuries dominate in triathlon. And while acute crashes on the bike or traumatic falls happen, the biggest threat to a triathlete’s season is the steady wear and tear of repetitive stress.
The Big Five: Most Common Triathlete Injuries
Let’s break down the five injuries I see most often in triathletes — their causes, symptoms, and what you can do about them.
1. Patellofemoral Pain Syndrome (PFPS) – The Classic “Runner’s Knee”
What it feels like:
A dull ache around or behind the kneecap, especially when running, sitting for long periods, squatting, or going down stairs.
Why it happens:
PFPS is usually the result of poor patellar tracking — the kneecap not gliding smoothly in its groove.
Common Triggers:
Tight hamstrings, quads, or IT band pulling on the knee
Weak glutes failing to stabilize hip and femur rotation
Foot pronation changing leg mechanics
Muscle imbalances between quads (especially weakness in the vastus medialis oblique)
How to fix it:
Mobility first: Stretch hamstrings, hip flexors, quads, calves, and IT band.
Targeted strength: Focus on VMO activation with quad sets and straight-leg raises. Build hip strength (glute medius and maximus).
Manual therapy: Soft tissue work, Graston, and patellar mobilizations help restore glide.
Modalities: Ice, compression, and electrical stimulation can help reduce inflammation.
Gradual return: Progress strength and function with controlled loading.
Recovery timeline: With proper treatment, many athletes see improvement in 6–12 weeks. The key is catching it early and not running through pain. According to McConnell, it only takes 20 ml of fluid/saline/swelling to inhibit proper contraction of the VMO. Proper rest is needed and RICE needs to be used properly by the triathlete.
These methods are important to improve blood flow and properly realign collagen fibers, scar tissue, and fascia surrounding the muscles. This will ultimately improve the triathlete's range of motion and flexibility, decreasing the forces going through the patellofemoral joint.
Electrical stimulation, specifically Russian electrical stimulation and pulsed-direct current from the Neubie Neufit, may also be used to promote proper contraction of the VMO.
A number of modalities such as Class IV Laser and GameReady (ice and compression) can also be used to promote healing and reduce inflammation in the knee joint and surrounding structures.
2. Iliotibial Band Syndrome (ITBS) – The Outer Knee Pain
What it feels like:
Sharp pain on the outside of the knee, sometimes radiating into the thigh or calf. Often flares up after a certain distance in a run.
Why it happens:
The IT band is a thick band of tissue running along the outside of the thigh. With repetitive flexion and extension (like running thousands of steps), it can rub against the femur, causing friction and inflammation. It has been estimated that knee flexion occurs approximately 800 times per mile of running.
Common Triggers:
Weak glutes leading to poor hip stability
Overstriding or poor running mechanics
Sudden mileage increases (especially >10% per week)
Tight IT band and surrounding structures
Worn-out shoes or improper footwear
Cycling in high gears for extended periods
How to fix it:
Strengthen the glutes: Especially the glute medius for hip control.
Stretch supporting structures: TFL, quads, and hips.
Cross-train and unload: Reduce aggravating mileage while maintaining fitness through swimming or cycling.
Manual therapy: Graston and soft tissue work (especially on the TFL rather than the band itself).
Address footwear: Replace shoes every 400–600 miles.
Recovery timeline: Most athletes improve within 4–6 weeks with consistent rehab. Compliance with strength and mobility work is the difference-maker.
A comprehensive stretching program will be utilized to improve the triathlete's range of motion and flexibility.
Applying the Graston techniques to the tensor fascia latae will also be beneficial to reduce the strain the iliotibial band has on the knee. Trying to perform soft tissue massage on the iliotibial band itself has shown to be unsuccessful. The tensor fascia latae muscle forms the iliotibial band as it travels distally along the lateral aspect of the thigh.
Electrical stimulation, GameReady, and the Normatec could also be used to reduce inflammation and reduce pain.
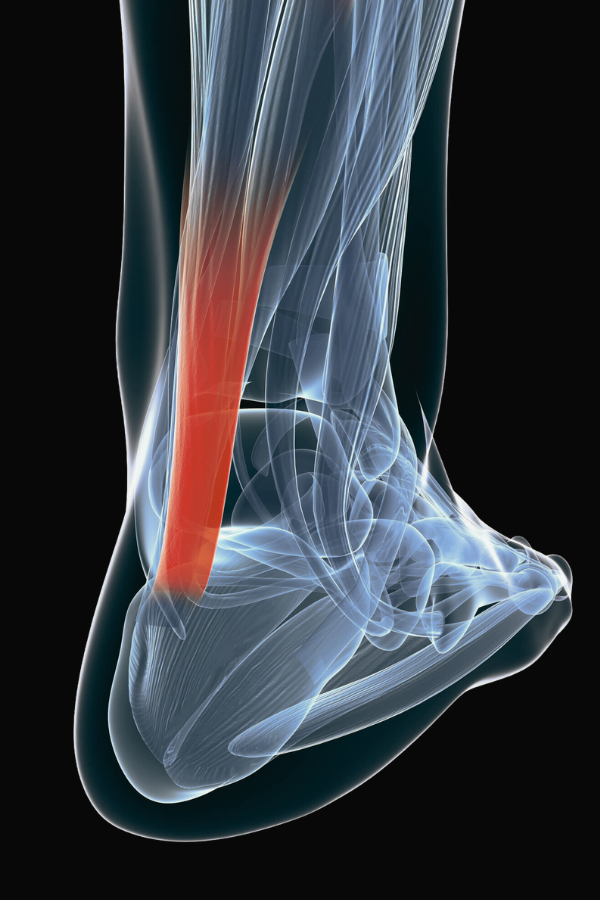
3. Achilles Tendonitis – The Overused Heel
What it feels like:
Pain and stiffness in the back of the heel or along the Achilles tendon, especially during push-off in running or cycling climbs.
Why it happens:
The Achilles absorbs massive loads during running — ranging from 5.3 to 10.0 times body weight (depending on speed, mechanics, individual differences). Overuse, poor footwear, or weak calves can create microtears that lead to chronic tendon pain.
Common Triggers:
Running hills or uneven surfaces
Sudden increases in mileage or intensity
Poor bike fit (toe clips too far forward)
Weak calves and soleus (especially eccentric strength)
Flat feet or excessive pronation
Tight calves limiting ankle mobility
How to fix it:
Unload the tendon: Heel lifts or temporary activity modification.
Control inflammation: Ice, compression, ultrasound, and soft tissue work.
Eccentric strengthening: Heel drops and soleus-focused strengthening are key.
Progress carefully: Begin with non-weight-bearing cardio (swimming, cycling), then gradually load tendon.
Manual therapy: Graston and massage help remodel scar tissue and realign collagen.
Recovery timeline: Achilles tendonitis can be stubborn — often 8–12+ weeks. But with consistent loading and patience, recovery is excellent.
4. Low Back Pain – The Cyclist’s Curse
What it feels like:
Dull ache, stiffness, or sharp nerve-like pain in the lower back, often during or after long bike sessions.
Why it happens:
Spending hours hunched in aero position puts huge demands on the spine.
Common Triggers:
Poor bike fit (seat too high, wrong reach, or improper handlebar setup)
Weak core and glutes failing to stabilize pelvis
Limited hip and thoracic mobility
Excessive lumbar flexion from aero position
Long hours without positional change
How to fix it:
Check bike fit: Seat height, saddle position, and reach must be dialed in.
Strengthen the core and glutes: Build endurance in stabilizers, not just brute strength.
Improve mobility: Hip flexors, hamstrings, and thoracic spine extension.
Manual therapy: Graston, active release, and traction can reduce pain.
Alter-G treadmill or pool running: Allows cardio training without spinal load.
Recovery timeline: Highly variable — some athletes bounce back in weeks, others need months of consistent work.
5. Shoulder Impingement – The Swimmer’s Setback
What it feels like:
Aching pain in the front or top of the shoulder, worse with overhead motion (especially swimming).
Why it happens:
Swimming requires thousands of overhead strokes, which narrows the space under the acromion and irritates tendons or bursa.
Common Triggers:
Weak scapular stabilizers
Poor posture or rounded shoulders
Overuse without recovery
Muscle imbalances between chest and back
How to fix it:
Scapular stability training: Strengthen lats, traps, and rotator cuff.
Improve posture: Thoracic extension mobility and postural awareness.
Gradual loading: Pain-free ROM and progressive resistance.
Manual therapy: Graston technique, massage, and mobilizations to reduce restrictions.
Modify swimming load: Avoid painful ranges until strength returns.
Recovery timeline: Most athletes recover in 6–10 weeks with proper strengthening and load management.
Injury Risks Across the Phases of a Triathlon
Injuries don’t just happen randomly — they often show up during specific phases of training.
Swimming Phase
Risk: Shoulder impingement, biceps tendon pain, low back from kicking
Prevention: Focus on technique, thoracic mobility, and shoulder endurance
Cycling Phase
Risk: Low back pain, neck strain, knee pain
Prevention: Proper bike fit, core/glute endurance, posture breaks during long rides
Running Phase
Risk: PFPS, ITBS, Achilles tendonitis, plantar fasciitis, stress fractures
Prevention: Gradual mileage increases, strength work, proper footwear, pacing strategy
How to Prevent Triathlon Injuries Before They Happen
The best injury treatment is prevention. Every triathlete should focus on:
Strength Training: Build balanced strength in hips, glutes, core, and upper back.
Mobility Work: Daily mobility for hips, hamstrings, calves, and shoulders.
Smart Programming: Avoid sudden mileage spikes and balance intensity with recovery.
Bike Fit & Equipment: Ensure shoes, saddle, and aerobars are set up for your body.
Recovery Practices: Sleep, nutrition, hydration, and active recovery are non-negotiable.
Final Thoughts: Train Smarter, Not Just Harder
Triathlon demands more from the body than almost any other sport. That’s why injury prevention isn’t just about surviving training — it’s about setting yourself up for long-term performance.
When you understand the most common injuries, recognize early warning signs, and put the right strength, mobility, and recovery strategies in place, you can stay healthy, keep building fitness, and show up on race day ready to perform.
And if you’re already dealing with one of these injuries, remember this: most triathlon injuries are highly treatable with the right plan. Don’t push through pain and hope it goes away. Address it now, so you don’t lose months of training later.
Ready to Take the Guesswork Out of Training?
If you’re serious about staying healthy and performing at your best, don’t wait until injury forces you to stop. I help triathletes and endurance athletes identify imbalances, fix mechanics, and create individualized plans that keep you training and racing strong.
References
Andersen C, Clarsen B, Johansen T, Engebretsen L. High prevalence of overuse injury among iron-distance triathletes. British Journal of Sports Medicine. 2013.
Wilk et al. Medical help-seeking among triathletes.
O’Toole et al. Low back pain and sciatica in triathletes.
Guezennec et al. Performance and injury risks in Olympic triathlon running phases.
Laird et al. Ultra-endurance triathlons: medical care visits and causes.